Frozen Shoulder
Subtitle: What to know about stiffness, motion limits, and supportive care.
Introduction
Frozen shoulder (also called adhesive capsulitis) is a condition where the shoulder becomes painful and increasingly stiff over time. Many people notice it when everyday tasks—like reaching into a cupboard or putting on a jacket—start to feel limited and uncomfortable. Symptoms may last for months, and sometimes longer, but the shoulder often gradually loosens with time and guided care.
This article explains how frozen shoulder is commonly described, what movement may feel like, and how care is usually approached. It also outlines how massage therapy may play a supportive comfort role alongside other options.
How This Condition Is Commonly Described
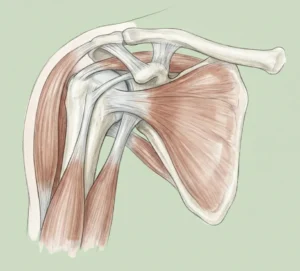
Frozen shoulder is often described as a gradual loss of shoulder motion with pain that can make the joint feel “stuck.” The shoulder joint capsule (the connective tissue around the joint) is commonly described as becoming tighter and less flexible, which can limit movement.
It may begin without a clear injury. In some cases, it shows up after a period of reduced use, such as after surgery or when the arm has been kept still for a while. Frozen shoulder is also more often discussed in people with certain health conditions (for example, diabetes), but it can happen to anyone.
How Movement, Pain, or Stiffness May Be Experienced
Pain often starts slowly and may be worse at night. As stiffness increases, reaching and rotating the arm can feel harder, even for small tasks. Some people notice that both “active” movement (moving your arm yourself) and “passive” movement (someone else gently moving it) feel limited.
Common daily-life examples: reaching behind your back to fasten a bra, putting on a seatbelt, or lifting your arm to wash your hair. You may also notice a protective “guarding” response, where the shoulder and neck tense up because the movement feels uncomfortable.
Frozen shoulder is often discussed in phases. Early on, pain can be more noticeable (“freezing”). Later, stiffness may be the main issue (“frozen”). Over time, movement may gradually return (“thawing”). The timeline varies between individuals.
 How Care Is Commonly Approached (General Overview)
How Care Is Commonly Approached (General Overview)
Care is usually focused on keeping the shoulder as functional as possible while respecting pain. A clinician may recommend a plan that includes guided exercises, activity adjustments, and symptom relief options. The goal is often to support comfortable movement and avoid long periods of complete rest.
Movement guidance: Gentle range-of-motion work is commonly suggested. This might include pendulum swings, light stretching, and controlled shoulder rotations. Many people do better with consistent, mild practice rather than pushing hard through pain.
Symptom support: Heat or cold may be used depending on what feels soothing. Over-the-counter pain relief may be discussed with a pharmacist or clinician based on your personal health history.
Medical options: Some people are offered injections or other procedures to help with pain and mobility, especially early on. Physical therapy is commonly recommended to support flexibility and function. If symptoms are persistent or very limiting, an orthopedic or rehab specialist may discuss additional options.
Massage Therapy’s Supportive Role
Massage therapy does not replace medical evaluation or a rehab plan. For frozen shoulder, massage is best thought of as a way to support comfort and help you feel more at ease in your body while you work on gentle movement.
Depending on the person and the phase of symptoms, sessions may focus on areas that often tighten when the shoulder is guarded—such as the neck, upper back, chest, and surrounding shoulder muscles. This may support relaxation and body awareness, which some people find helpful when returning to comfortable movement.
In practice, a massage therapist may use lighter pressure at first, check in often, and avoid forcing the shoulder into painful positions. Many people prefer shorter, more comfortable sessions rather than intense work that leaves the area sore or irritated.
Safety Considerations & When to Seek Professional Care
It’s smart to get assessed if shoulder pain or stiffness is new, worsening, or interfering with sleep and daily tasks. Frozen shoulder can look similar to other shoulder problems, and a clinician can help rule out other causes and guide next steps.
Seek urgent care if: pain follows a fall or injury, the shoulder looks deformed, you cannot use the arm at all, you have fever with redness/warmth, or you notice new numbness, tingling, or weakness in the arm or hand.
For massage, share your health history and current symptoms. If you have conditions that affect sensation, circulation, or tissue healing (such as diabetes), or if you’re on blood thinners, ask your clinician whether massage is appropriate and let your therapist know so pressure and positioning can be adjusted.
Key Takeaways
- Frozen shoulder is commonly described as pain plus a gradual loss of motion.
- Night discomfort and difficulty reaching behind the back are common complaints.
- Gentle, consistent movement is often preferred over pushing through sharp pain.
- Massage may support comfort, relaxation, and reduced guarding alongside guided exercise.
- Get checked if symptoms are severe, sudden, or linked to injury or concerning signs.
FAQs
How long does frozen shoulder usually last?
Many people notice that symptoms change over time and may last months to years. Some sources describe improvement often occurring within about 1 to 3 years, but timelines vary between individuals. Your overall health, activity level, and how early you start guided movement may influence the experience.
How can I tell if it is a Frozen Shoulder or something else?
Several shoulder issues can cause pain and limited movement, including tendon or rotator cuff problems. A clinician can assess your range of motion, your history, and whether imaging is needed. It’s especially important to get checked if symptoms started after an injury.
Should I keep moving my shoulder if it hurts?
In many cases, gentle movement within tolerable limits is commonly recommended. The aim is often to stay active without forcing painful ranges. A physical therapist can help you find the right level and choose exercises that match your symptoms.
Can massage therapy help with frozen shoulder?
Massage may support relaxation, comfort, and reduced muscle guarding around the shoulder and upper back. It’s usually most helpful when paired with a movement plan guided by a clinician or physical therapist. A good session should feel tolerable during and after, not like it “pushes through” sharp pain.
When should I see a healthcare professional?
Consider an evaluation if stiffness and pain are worsening, disrupting sleep, or limiting daily tasks. Seek urgent care for severe pain after trauma, visible deformity, fever with redness/warmth, or new numbness or weakness. Getting guidance early can help you choose safe next steps.
Many people notice that symptoms change over time and may last months to years. Some sources describe improvement often occurring within about 1 to 3 years, but timelines vary between individuals. Your overall health, activity level, and how early you start guided movement may influence the experience.
Several shoulder issues can cause pain and limited movement, including tendon or rotator cuff problems. A clinician can assess your range of motion, your history, and whether imaging is needed. It’s especially important to get checked if symptoms started after an injury.
In many cases, gentle movement within tolerable limits is commonly recommended. The aim is often to stay active without forcing painful ranges. A physical therapist can help you find the right level and choose exercises that match your symptoms.
Massage may support relaxation, comfort, and reduced muscle guarding around the shoulder and upper back. It’s usually most helpful when paired with a movement plan guided by a clinician or physical therapist. A good session should feel tolerable during and after, not like it “pushes through” sharp pain.
Consider an evaluation if stiffness and pain are worsening, disrupting sleep, or limiting daily tasks. Seek urgent care for severe pain after trauma, visible deformity, fever with redness/warmth, or new numbness or weakness. Getting guidance early can help you choose safe next steps.
Sources
NHS. (n.d.). Frozen shoulder. https://www.nhs.uk/conditions/frozen-shoulder/
Mayo Clinic. (2022). Frozen shoulder – Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/frozen-shoulder/symptoms-causes/syc-20372684
Mayo Clinic. (2022). Frozen shoulder – Diagnosis and care. https://www.mayoclinic.org/diseases-conditions/frozen-shoulder/diagnosis-treatment/drc-20372690
American Academy of Orthopaedic Surgeons. (n.d.). Frozen Shoulder – Adhesive Capsulitis. https://orthoinfo.aaos.org/en/diseases–conditions/frozen-shoulder
National Center for Complementary and Integrative Health. (n.d.). Massage Therapy: What You Need To Know. https://www.nccih.nih.gov/health/massage-therapy-what-you-need-to-know
“This article is for informational and educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare professional before starting or changing any health or wellness practice.
Illustrations used in this article are for educational purposes only and may be AI-generated. They are not intended to diagnose or represent medical conditions.”